Gestational Diabetes
Diabetes - Gestational
Introduction
Gestational Diabetes is the most common pregnancy complication. Diabetes is a disease that affects how the body uses glucose, a sugar that is a source of fuel. Normally, insulin, a hormone, helps glucose get into the body cells where it is used for energy. Women with Gestational Diabetes either do not produce enough insulin or the insulin does not work like it should. As a result, glucose does not get into the body cells. Too much sugar in the blood can make people ill and result in medical complications.
There are different types and causes of diabetes. Gestational Diabetes is a temporary condition that occurs in a small percentage of women during pregnancy. Uncontrolled Gestational Diabetes is dangerous to both the mother and the fetus. However, when blood glucose levels are closely controlled, women with Gestational Diabetes can have healthy pregnancies and healthy babies.
Anatomy
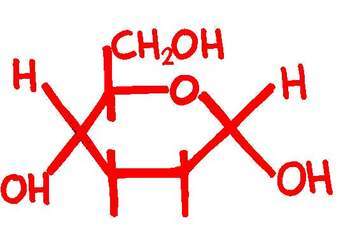
Your body is composed of millions of cells. The cells need energy to function. One way the cells receive energy is from the food that you eat. Whenever you eat or drink, some of the food is broken down into glucose. Glucose is a sugar that is released into your blood. It is a major source of energy for your body cells. Glucose is transported from your bloodstream and into your cells with the help of insulin.
Insulin is a hormone that is produced by the beta cells in your pancreas. Your pancreas is a gland located near your stomach that produces chemicals for food digestion. Insulin regulates the amount of glucose in your blood in a continual process. When you eat, the amount of glucose in your bloodstream rises. In response to the elevated blood glucose level, your beta cells produce insulin. The insulin moves the glucose out of the bloodstream and into your cells. In turn, a lower level of glucose is left in the blood stream. To prevent your blood glucose level from getting too low, your body signals you to eat. This starts the process again so that your body cells continually receive the energy that they need.
Causes
Gestational Diabetes occurs in a small percentage of pregnant women. The placenta, which supports the baby, produces hormones to help the baby develop. However, Gestational Diabetes results when the hormones produced by the placenta cause insulin resistance in the mother. Insulin resistance makes it difficult for her body to use the insulin that she produces. She may need to up to three times as much insulin because her body does not recognize or respond to the insulin that is produced. As a result, glucose is unable to get into the cells for energy. The glucose accumulates in the blood and causes high blood glucose levels. This condition is called hyperglycemia.
Gestational Diabetes develops most frequently during the last three months of pregnancy, when the baby’s body has been formed. Because Gestational Diabetes generally occurs later in pregnancy, it does not cause the type of birth defects associated with mothers that had diabetes before pregnancy. However, untreated or poorly controlled Gestational Diabetes can harm both the mother and the baby. Gestational Diabetes usually does not continue after pregnancy.
Symptoms
Frequent urination, excessive hunger, and excessive thirst are symptoms that suggest Gestational Diabetes. This happens as your body tries to remove the excess blood sugar by passing it out of your body in urine. In turn, you feel extremely thirsty. Because your body is not getting energy from blood sugar, it signals you to eat a lot. You may feel tired and weak because your body cells cannot use glucose for energy.
Diagnosis
It is important that you tell your doctor the symptoms you experience and discuss your concerns. Women with a high risk for Gestational Diabetes should be screened as early as possible during their pregnancies. For these women, a normal screening test should be followed by a repeat test between the 24th and 28th week of pregnancy. All other women should be screened between the 24th and 28th week of pregnancy. Your doctor can diagnose Gestational Diabetes by testing your urine and blood.
Your doctor will test your urine for glucose and ketones. Ketones are acids that accumulate in the blood and appear in urine when the body does not have enough insulin. The tests are simple to conduct. Test strips are simply placed in your urine sample. Your doctor will read the results after a short period of time.
Your doctor can also determine if you have diabetes by conducting blood glucose tests. The Fasting Plasma Glucose Test (FPG) or the Oral Glucose Tolerance Test (OGTT) are commonly used. The FPG measures blood glucose levels after you have fasted or not eaten for a period of time. The OGTT test measures blood glucose levels after fasting and again a few hours after you drink a high-glucose beverage. The FPG and the OGTT test indicate your blood glucose level for one time on a given day.
Because blood glucose levels fluctuate from day to day, your doctor can also test how your blood glucose levels have been over a period of three months. To do so, your doctor will use an A1C test, also called glycated hemoglobin or HbA1c test. The A1C test measures how much extra glucose has glycated or attached to your red blood cells over the last 120 days, the lifespan of a red blood cell.
Treatment
You need to follow your doctor’s instructions for carefully monitoring your blood glucose levels. You will need to check your blood glucose levels throughout the day. Your doctor will help you establish a schedule. Make sure that you write down the time that you tested your blood and the result. Bring your logbook to each of your doctor appointments.
To test your blood glucose, you will prick your finger with a small sharp needle. You will place a drop of blood on a test strip. A glucose meter will display your results.
Depending on the results of your blood test, you may need to inject yourself with insulin. The insulin will help to control your blood glucose levels. Your doctor will let you know how much insulin to use. It will depend on your weight, what you eat, and how active you are. As your pregnancy progresses, the placenta will produce more hormones, and you may need to use more insulin. Your doctor will let you know how much more to use, based on the records in your logbook.
You may also need to check your urine, according to your doctor’s instructions. You should test your urine for ketones when your blood glucose level is high. Urine testing involves placing test strips in your urine sample and reading the results after a short period of time.
Managing Gestational Diabetes also includes a nutritional component. Your doctor or a registered nutritionist can help you plan what to eat to help regulate your blood glucose levels and weight. It can be helpful to eat several small meals throughout the day. Your health care professional can help you learn to make good food selections, read nutrition labels, measure portion sizes, and plan well-balanced meals.
Exercise is another important element for managing Gestational Diabetes. Exercise may help to lower your blood glucose level, blood pressure, and cholesterol. It also may help your body to use insulin better. All pregnant women should consult with their doctor prior to beginning an exercise program. Your doctor will let you know how much to exercise and the type of exercises that are safe for you.
In addition to managing your blood sugar, eating smart, and exercising, you should also maintain appropriate cholesterol and blood pressure levels. It is important not to smoke. Not only is smoking unhealthy for your developing baby, but smoking can also increase blood sugar levels and contribute to the development of medical complications.
Treatment for Gestational Diabetes can prevent symptoms from happening. However, even with treatment, some problems associated with Gestational Diabetes may occur. These conditions include hyperglycemia, ketoacidosis, and hypoglycemia.
Hyperglycemia, also called high blood glucose, happens occasionally to people with diabetes. Untreated hyperglycemia can lead to medical complications. Hyperglycemia can occur for many reasons. Women with Gestational Diabetes may experience it if their body is not using insulin effectively, if they do not have enough insulin, or if they ate more than planned and exercised less than planned.
The warning signs and symptoms of hyperglycemia include high blood glucose levels, high levels of sugar in the urine, frequent urination, and increased thirst. You should follow your doctor’s instructions for treating hyperglycemia as soon as you detect high blood sugar levels or ketones in your urine—this is very important. If you fail to do so, ketoacidosis could occur. If you have ketones in your urine, do not exercise. Exercising will only make the situation worse.
Ketoacidosis is a serious condition—it can lead to diabetic coma or death. Ketones are acids that accumulate in the blood when your body breaks down fats. Your body releases ketones through urine. Ketones appear in urine when the body does not have enough insulin. Ketoacidosis occurs when all of the ketones cannot be released through urine and the amount of ketones remaining in the blood becomes high enough to poison the body. Ketoacidosis usually develops slowly, but when vomiting occurs, the condition can develop in just a few hours.
The first symptoms of ketoacidosis include thirst, dry mouth, frequent urination, high blood glucose levels, and high levels of ketones in the urine. These symptoms are followed by dry or flushed skin; continual tiredness; nausea, abdominal pain, or vomiting; difficulty breathing; impaired attention span or confusion; and fruity smelling breath. If you have any of the symptoms contact your doctor immediately; call emergency services, usually 911; or go to the nearest emergency room. Treatment for ketoacidosis usually involves a hospital stay.
You can help prevent ketoacidosis by monitoring yourself for warning signs and checking your urine and blood regularly. Follow your doctor’s instructions if you detect high levels of ketones. If you have high levels of ketones, do not exercise. Exercise increases the levels of ketones.
Hypoglycemia, also called low blood sugar or insulin reaction, is not always preventable. Hypoglycemia can occur even if you do everything that you can to manage your diabetes. Symptoms of hypoglycemia include shakiness, dizziness, sweating, hunger, headache, pale colored skin, sudden moodiness, clumsiness, seizure, poor attention span, confusion, and tingling sensations around your mouth.
Check your blood if you suspect that your blood glucose level is low. You should treat hypoglycemia immediately. The quickest way to treat hypoglycemia is to raise your blood sugar level with some form of sugar—glucose tablets, fruit juice, or hard candy. Ask your doctor for a list of appropriate foods. Once you have checked your blood glucose level and treated your hypoglycemia, repeat the process again until your signs and symptoms have cleared.
It is important to treat hypoglycemia immediately or you could pass out. If you pass out, you need immediate treatment. You should receive an injection of glucagon. Glucagon is a medication that raises blood sugar. You should tell those around you how and when to use it. If glucagon is not available, you need emergency medical assistance. Someone should take you to the emergency room or call emergency medical services, usually 911. If you pass out from hypoglycemia, you should not inject insulin or consume food or fluids.
Usually, blood glucose levels return to normal following the childbirth. This is because the placenta, which was producing the hormones that caused insulin resistance, is delivered. Your doctor will check to make sure that your blood sugar levels have returned to normal. Additionally, your doctor will test you for diabetes several weeks after your delivery. You should also be tested for Type 2 Diabetes in the future. Women who develop Gestational Diabetes during pregnancy are at a higher risk for developing Type 2 Diabetes as they age.
The insulin will help to control your blood glucose levels. Your doctor will let you know how much insulin to use. It will depend on your weight, what you eat, and how active you are. As your pregnancy progresses , the placenta will produce more hormones, and you may need to use more insulin. Your doctor will let you know how much more to use, based on the records in your logbook.
You may also need to check your urine, according to your doctor’s instructions. You should test your urine for ketones when your blood glucose level is high. Urine testing involves placing test strips in your urine sample and reading the results after a short period of time.
Managing Gestational Diabetes also includes a nutritional component. Your doctor or a registered nutritionist can help you plan what to eat to help regulate your blood glucose levels and weight. It can be helpful to eat several small meals throughout the day. Your health care professional can help you learn to make good food selections, read nutrition labels, measure portion sizes, and plan well-balanced meals.
Exercise is another important element for managing Gestational Diabetes. Exercise may help to lower your blood glucose level, blood pressure, and cholesterol. It also may help your body to use insulin better. All pregnant women should consult with their doctor prior to beginning an exercise program. Your doctor will let you know how much to exercise and the type of exercises that are safe for you.
In addition to managing your blood sugar, eating smart, and exercising, you should also maintain appropriate cholesterol and blood pressure levels. It is important not to smoke. Not only is smoking unhealthy for your developing baby, but smoking can also increase blood sugar levels and contribute to the development of medical complications.
Treatment for Gestational Diabetes can prevent symptoms from happening. However, even with treatment, some problems associated with Gestational Diabetes may occur. These conditions include hyperglycemia, ketoacidosis, and hypoglycemia.
Hyperglycemia, also called high blood glucose, happens occasionally to people with diabetes. Untreated hyperglycemia can lead to medical complications. Hyperglycemia can occur for many reasons. Women with Gestational Diabetes may experience it if their body is not using insulin effectively, if they do not have enough insulin, or if they ate more than planned and exercised less than planned.
The warning signs and symptoms of hyperglycemia include high blood glucose levels, high levels of sugar in the urine, frequent urination, and increased thirst. You should follow your doctor’s instructions for treating hyperglycemia as soon as you detect high blood sugar levels or ketones in your urine—this is very important. If you fail to do so, ketoacidosis could occur. If you have ketones in your urine, do not exercise. Exercising will only make the situation worse.
Ketoacidosis is a serious condition—it can lead to diabetic coma or death. Ketones are acids that accumulate in the blood when your body breaks down fats. Your body releases ketones through urine. Ketones appear in urine when the body does not have enough insulin. Ketoacidosis occurs when all of the ketones cannot be released through urine and the amount of ketones remaining in the blood becomes high enough to poison the body. Ketoacidosis usually develops slowly, but when vomiting occurs, the condition can develop in just a few hours.
The first symptoms of ketoacidosis include thirst, dry mouth, frequent urination, high blood glucose levels, and high levels of ketones in the urine. These symptoms are followed by dry or flushed skin; continual tiredness; nausea, abdominal pain, or vomiting; difficulty breathing; impaired attention span or confusion; and fruity smelling breath. If you have any of the symptoms contact your doctor immediately; call emergency services, usually 911; or go to the nearest emergency room. Treatment for ketoacidosis usually involves a hospital stay.
You can help prevent ketoacidosis by monitoring yourself for warning signs and checking your urine and blood regularly. Follow your doctor’s instructions if you detect high levels of ketones. If you have high levels of ketones, do not exercise. Exercise increases the levels of ketones.
Hypoglycemia, also called low blood sugar or insulin reaction, is not always preventable. Hypoglycemia can occur even if you do everything that you can to manage your diabetes. Symptoms of hypoglycemia include shakiness, dizziness, sweating, hunger, headache, pale colored skin, sudden moodiness, clumsiness, seizure, poor attention span, confusion, and tingling sensations around your mouth.
Check your blood if you suspect that your blood glucose level is low. You should treat hypoglycemia immediately. The quickest way to treat hypoglycemia is to raise your blood sugar level with some form of sugar—glucose tablets, fruit juice, or hard candy. Ask your doctor for a list of appropriate foods. Once you have checked your blood glucose level and treated your hypoglycemia, repeat the process again until your signs and symptoms have cleared.
It is important to treat hypoglycemia immediately or you could pass out. If you pass out, you need immediate treatment. You should receive an injection of glucagon. Glucagon is a medication that raises blood sugar. You should tell those around you how and when to use it. If glucagon is not available, you need emergency medical assistance. Someone should take you to the emergency room or call emergency medical services, usually 911. If you pass out from hypoglycemia, you should not inject insulin or consume food or fluids.
Usually, blood glucose levels return to normal following the childbirth. This is because the placenta, which was producing the hormones that caused insulin resistance, is delivered. Your doctor will check to make sure that your blood sugar levels have returned to normal. Additionally, your doctor will test you for diabetes several weeks after your delivery. You should also be tested for Type 2 Diabetes in the future. Women who develop Gestational Diabetes during pregnancy are at a higher risk for developing Type 2 Diabetes as they age.
Prevention
You should wear a MedicAlert bracelet and carry a MedicAlert card in your wallet. In the case of an emergency, the MedicAlert information will be helpful to the medical professionals treating you.
Women who had Gestational Diabetes during pregnancy have an increased risk for developing Type 2 Diabetes in the future. These women should discuss their concerns with their doctors and be screened for Pre-Diabetes and Type 2 Diabetes. People may reduce their risk of developing Type 2 diabetes by maintaining a healthy weight, exercising, and eating healthy.
Additionally, women that had Gestational Diabetes during pregnancy are at risk for developing it again in future pregnancies. Women that are planning on getting pregnant again should talk with their doctor. Making lifestyle changes before the next pregnancy may be helpful.
Am I at Risk
Many women who develop Gestational Diabetes have no known risk factors. Women who are
members of ethnic minority groups including African Americans, Native Americans, Hispanics,
Latinos, Asians, and Pacific Islanders develop Gestational Diabetes more frequently than
Caucasians. The following factors appear to increase the risk of developing Gestational Diabetes during pregnancy:
_____ A family history of diabetes is associated with an increased chance of developing Gestational Diabetes. If your parents, brothers, or sisters have diabetes your risk increases.
_____ Women that had Gestational Diabetes with a previous pregnancy are at risk for developing it with each future pregnancy.
_____ Women that are overweight before they become pregnant have an increased risk of developing Gestational Diabetes when they are pregnant.
_____ Having glucose in your urine, an impaired glucose tolerance, or impaired fasting glucose tolerance are risk factors for diabetes.
_____ Polyhydramnios, a condition when you have too much amniotic fluid, is a risk factor for diabetes.
_____ Previously giving birth to a stillborn baby or a baby that weighed more than nine pounds increases your risk for Gestational Diabetes during pregnancy.
Complications
Untreated or poorly controlled Gestational Diabetes can harm both the mother and the baby. The mother is at risk for hyperglycemia, ketoacidosis, and hypoglycemia, as explained above. Mothers with Gestational Diabetes need to maintain their blood glucose levels. By doing so, she ensures a healthy pregnancy and delivery.
Because Gestational Diabetes generally occurs later in pregnancy, it does not cause the type of birth defects associated with mothers that had diabetes before pregnancy. However, high blood glucose levels in the mother can affect the baby during development and after delivery.
If your blood glucose levels are out of control during pregnancy, the extra glucose can travel across the placenta and to your developing baby. In turn, the baby’s blood glucose level rises. This causes the developing baby to produce more insulin to get rid of the extra blood glucose. The excess glucose is stored as fat in the baby. The excess fat can lead to a condition called macrosomia, making the baby larger than normal.
Babies with macrosomia have an increased risk for damage to their shoulders during birth, breathing problems, and very low blood glucose levels at birth. Your baby’s blood glucose level will be tested immediately after birth. If your baby’s blood glucose level is low, your baby will be given sugar water and sent to the neonatal intensive care unit for observation for a short period of time. The medical staff will monitor the baby for signs of a low blood glucose reaction.
Babies with mothers who had Gestational Diabetes have a higher risk of developing jaundice. Jaundice is a yellow discoloration of the skin, eyes, and mucous membranes. Jaundice occurs when there is too much bilirubin in the baby’s blood. Bilirubin is released when too many red blood cells accumulate in the blood. Jaundice can be treated in a few days with light therapy. Light therapy involves exposing your baby to special lights for select periods throughout the day and night.
Babies with mothers who had Gestational Diabetes also have a higher risk for developing diabetes in the future. Babies with excess insulin are at risk for childhood obesity. Additionally, mothers that experienced Gestational Diabetes during one pregnancy have an increased risk for developing it again in future pregnancies. Further, mothers that experienced Gestational Diabetes have an increased risk for developing Type 2 Diabetes years later. People with Type 2 Diabetes produce insulin, but they either do not produce enough or the insulin does not work like it should. People with Type 2 Diabetes need to diligently manage their disease to remain healthy and reduce the risk of medical complications.
Again, Gestational Diabetes usually ceases shortly after delivery. However, for a few women, pregnancy uncovers Type 1 or Type 2 Diabetes. In some cases, it may be difficult to determine exactly what form of diabetes a woman has during pregnancy. After delivery, women with Type 1 or Type 2 Diabetes will need to continue treatment for diabetes.
Advancements
Prevention, technology, and research have greatly improved the management of this diabetes. Sugar-free foods and new medicines have made diabetes management more convenient. New forms of insulin include fast-acting insulin and 24-hour forms. Further, insulin administration is easier with pens, pumps, and inhalers.